This policy brief was originally published in Japanese as part of a series of papers produced by a joint research project conducted by the Japan Center for International Exchange (JCIE) and the Tokyo University Institute for Future Initiatives (IFI) to provide analyses on global and regional health governance systems and structures and to offer concrete recommendations about the role Japan should play in the field of global health.
People often discuss the search for a “balance between preventing the spread of infection and maintaining socioeconomic activities.” But is there really a trade-off between these two concepts? In this article, I will summarize the relationship between infectious disease countermeasures and the economy, and then discuss the current challenges that are being addressed scientifically.
Infection Status and Determining Factors in Asia
The cumulative number of deaths from COVID-19 in countries in the Asian region total 874,198, which equates to 2.7 deaths per 10,000 people. The region has been much less affected than other regions, such as Europe (15 per 10,000) and North America (16 per 10,000).1 Different hypotheses have been proposed as the primary factors for this, such as the BCG vaccine theory or the cross-immunity theory (in which previous infection with a less virulent virus that is similar to COVID-19 prevents people infected with COVID-19 from developing worse symptoms), but research to date has refuted these hypotheses. Using the data that has been accumulated to date, we verified a number of key factors that have had the greatest relevance.2 (It should be noted that it is difficult to make comparisons between different countries as the definitions of number of deaths and the number of infected people vary. Differences in vaccination rates and the impact of variants on infection patterns are not taken into account.)
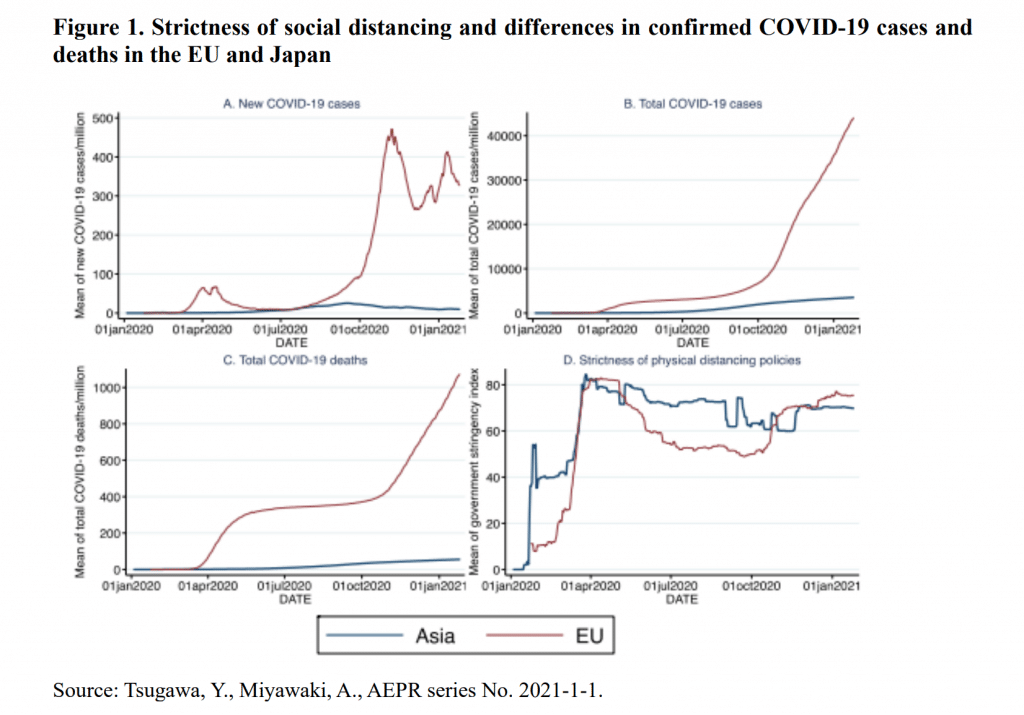
The first key factor we can point to is public health interventions (nonpharmaceutical interventions, or NPIs), such as lockdowns, school closures, social distancing, and mask wearing, which have been nearly continuously in place in Asia since early 2020, at which time there were few cases of infection. By contrast, NPIs in the European Union (EU) started around March, and these measures were eased in the summer of that year (see fig. 1). While there have been media reports that have repudiated the effect of lockdowns, all research studies have produced empirical data that show NPIs to be clearly effective as infection control measures.
The second key factor is that Asia is made up of many island countries, meaning that in comparison to land-based nations, where foreign nationals are able to enter the country by land, the effectiveness of border control measures at ports and airports can be seen more clearly.
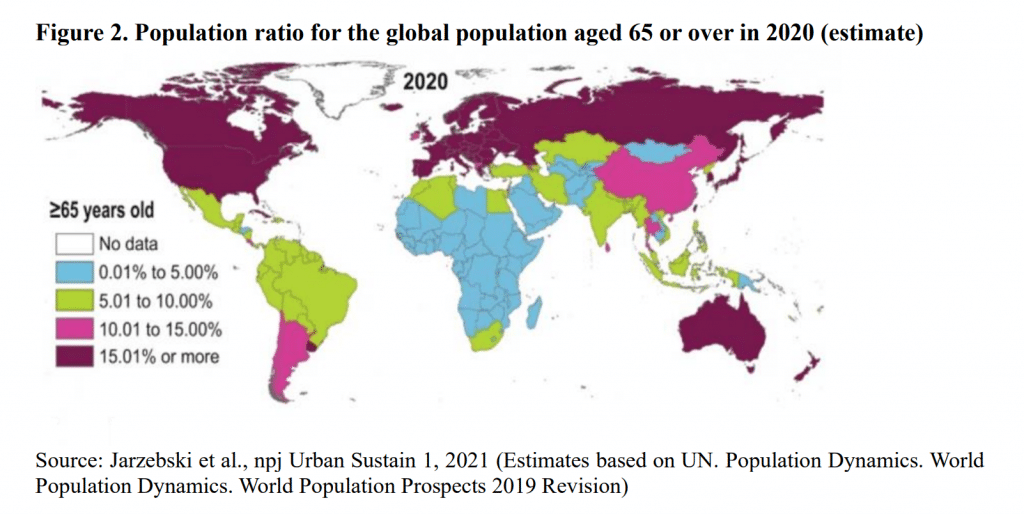
The third key factor is that the population in Asia is younger compared with Europe and the United States. COVID-19 does not often cause severe illness in young people (i.e., people under the age of 65), and most Asian countries (with the exception of Japan) have younger populations than European countries and the United States. In terms of the proportion of people over 65 years old, it is less than 10 percent in the majority of Asian countries (see fig. 2), except for Japan, which has the one of the most aged populations in the world.
Impact of Infectious Disease Measures on Economic Activity
The global economic impact of COVID-19 is estimated to be -4.5 percent of GDP, with losses of more than approximately ¥430 trillion. This figure is at a similar level to the impact of the 1918 influenza pandemic, but the mechanism behind this is said to be different. The period in which the 1918 pandemic occurred was a time of labor-intensive industrial structures, and the deaths of many people led to a drop in the global working population, while a drop in supply volume led to inflation, thereby leading to economic decline. In the current pandemic, it is said that the economic impact is due to a decrease in demand, with consumers not going out or buying things. However, it is hard to say sweepingly whether this is attributable to the lockdowns or whether economies will recover once countries reopen. Moreover, COVID-19 has not suppressed economic activity in all sectors. In-person service industries, such as restaurants and travel, have suffered a significant impact. However, new industries such as online businesses and delivery services have emerged, and economic strength can vary according to whether or not there is a transformation to such new industries. Saying that a lockdown stops all economic activities is too simplistic an argument, and the concept of running an economy without raising the risk of infection is important.
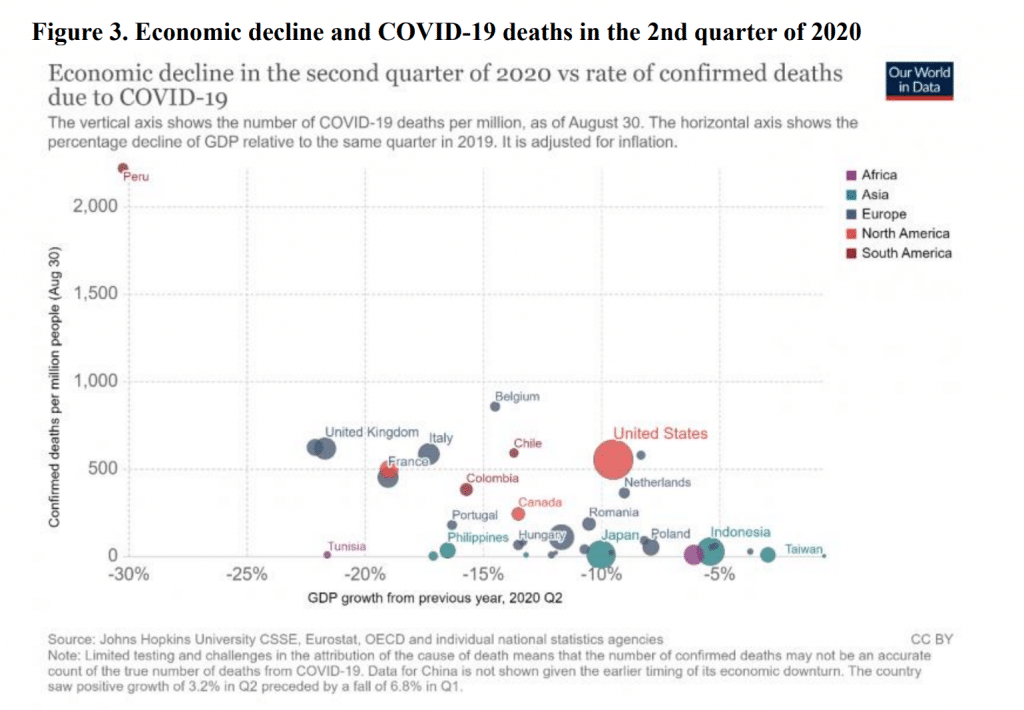
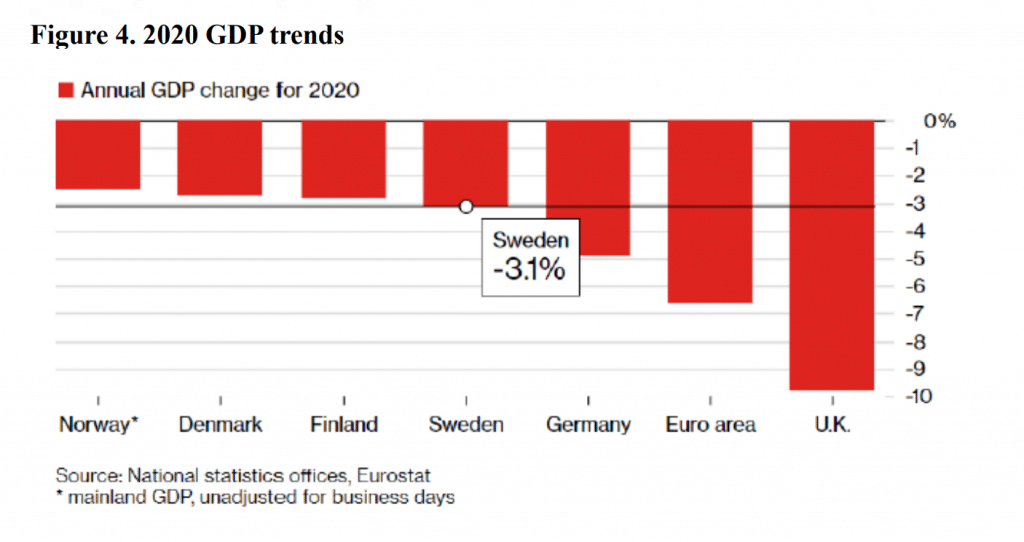
In Japan, there has actually been a tendency for infection cases to fall before the declaration of a state of emergency. It is possible that as people learned of rising rates from media reports, etc., it had a psychological impact that led to behavioral changes, such as people voluntarily staying home, and that in turn contributed to a lowering of the infection rates. If those countries with intensive pandemic countermeasures are the ones experiencing adverse effects on their economies, then there should be a positive correlation between GDP growth rate and the number of COVID-19 cases, but actually there is an inverse correlation (see fig. 3). While this is just a correlation, and the causal relationship is not known, there is no evidence that an economy will decline in proportion to the pandemic countermeasures that are taken. It is possible that measures to curb the spread of the virus could indeed be economic measures as well. If we take a look at Sweden, a nation that did not implement NPIs, the number of cases is naturally higher than in the surrounding Nordic countries, but there is not a substantial difference in terms of economic losses (see fig. 4). The main reasons for this are thought to be behavioral changes, such as elderly people staying home out of fear of infection, and that economic losses occurred due to trade, in a similar manner to what was happening in other countries. If Sweden did not implement any NPI measures, and not only had deaths but also suffered economic losses, then there would be scope for considering whether Swedish policies were appropriate. In fact, there is no trade-off between infection control and the economy, and this suggests the possibility that in a situation of rising case numbers, the economy cannot work without controlling infection (infections are upstream and the economy downstream).
The impact on the real economy, such as rising unemployment and bankruptcy rates, will be clearer in the future, but many countries are at present experiencing smaller than expected economic losses. In the United States, the real economy is said to be catching up, and some have expressed the optimistic viewpoint that there will not be a serious recession. In terms of the cost of economic and financial measures, the economic stimulus measures implement to date have been on an unprecedented scale, and consequently, economies have not ground to a halt. Moreover, although people were expecting a dramatic stock crash around March of last year, stock prices have been steadily rising ever since. For example, economic conditions, particularly in the IT industries, are improving in the United States and it could be said that the economic situation is not that bad from a macro perspective.
Limitations and Improvements to Existing Analytical Methods
In the field of health economics, health technology assessment (HTA) is a method for completely and comprehensively evaluating medical technology, incorporating medical, economic, and social impacts. Unfortunately, however, the COVID-19 pandemic has been an unprecedented event in which public health has directly impacted economies, and this impact has far surpassed the capacity of HTA analysis. For example, when we look at the cost-benefit of COVID-19 vaccines, it is impossible to calculate that with any real accuracy unless we look not only at the efficacy in terms of disease prevention and the prevention of serious illness but also calculate the macroeconomic impacts in such areas as the movement of people and trade. However, we believe that HTA does not calculate for externalized macroeconomic economic losses in terms of the methodology, and it underestimates productivity losses. Research to date has shown that a COVID-19 vaccine costs approximately US$8,200 per person (<$100,000- 150,000 per QALY is generally seen as a cost-effective intervention) to extend healthy life expectancy by one year (1 QALY), 3 however this is believed to be a considerable underestimate. The same can be said of the NPI cost-benefit analysis. Although there is no causal relationship between NPI deployment and economic impact, at present it is difficult to scientifically prove that NPI, which is low-cost and proven to be effective for preventing infections, represents the most cost-effective toolbox of measures.
In addition, it is crucial to take into account economic losses caused by the time taken for the development and roll-out of vaccines. Usually it takes 10 years to develop a vaccine (four years for the mumps vaccine, which is the fastest vaccine to have ever been developed), but vaccines for COVID-19 were developed within an unprecedented time of less than one year. If we think about how high the economic losses would have been if it had taken two years to develop a vaccine, then even if the impact on health is ignored and we only consider the economic returns, that could conceivably reduce the cost. However, it is hard to include these kinds of economic effects in an analysis using HTA in its current form.
COVID-19 should serve as an alarm bell, particularly for developed countries that have reduced investment in healthcare and public health due to their overconfidence that infections can be controlled with medicine (antibiotics, vaccines, etc.). In addition, while medicine and the economy have historically been viewed separately, it is clear that these healthcare and public health can cause substantial damage on the downstream economies at a global level. In developed countries in particular, medical expenses have been seen as a cost, but given that infectious diseases, such as the current pandemic, are expected to occur frequently in the future, there is a need to view infectious disease–related healthcare and public health as an investment from the perspective of economic measures and national defense, and consider how best to implement public policy measures. To do so will require that we bring together the collective knowledge of various research fields, improve methodologies such as the HTA to facilitate cost-benefit analyses that take into account macroeconomic contributions, and enable science to propose optimal measures that also reflect the macro-level impact.
About the Author
Yusuke Tsugawa is an Associate Professor at the UCLA David Geffen School of Medicine & Fielding School of Public Health.
Notes
- Calculated based on World Meter's coronavirus number of deaths and the population as of 2018 according to World Statistics 2000.
- Yusuke Tsugawa and A. Miyawaki, “Health and Public Health Implications of SARS/MARS/COVID-19 in Asian Countries,” JCER Working Paper, AEPR series, no. 2021-1-1.
- Michele Kohli, et al., “The Potential Public Health and Economic Value of a Hypothetical COVID19 Vaccine in the United States: Use of Cost-Effectiveness Modeling to Inform Vaccination Prioritization,” Vaccine 39, no. 7 (12 Feb 2021):1157–64, doi: 10.1016/j.vaccine.2020.12.078. Epub 2021 Jan 6.